This month is Stress Awareness Month which has been held every April for the last thirty years, yet events over the last two years have made this event even more essential. Anxieties over COVID and the impact of lockdowns have all taken a toll on our mental health. Multiple studies have shown a major increase in the number of adults reporting symptoms of anxiety, depression, and insomnia.
For those undergoing IVF, however, this has been an even more stressful time, with cancelled appointments, delayed procedures and worries about how the pandemic would impact their fertility treatment. We take a look at where stress, diet and fertility intersect.
Stress and the body
There are many factors that are stressful for mind and body – external pressures such as your job or family responsibilities and internal influences such as our diet or how body is functioning.
Stress affects our body in a myriad of ways: it increases blood pressure levels, spikes our blood sugar, releases stress hormones, and speeds up our heart as we enter a flight or fight response. The problem is that the pressure of modern-day living means we’re continually in a state of full alert.
Diet and fertility stress
A well-balanced diet can help us combat the physiological changes caused by stress. Much of the focus is on stabilising our blood sugar levels.
Prioritising protein: when the body is chronically stressed, it demands protein as that slows down release of sugar into the blood stream and the best sources are lean meat, fish, eggs, beans, pulses, nuts and seeds.
Time your intake: eating regular, well-balanced meals are the key to maintaining energy levels and your mood while staving off tiredness.
Fight the easy fix: highly refined foods such as white bread, pasta, sweets, cereals, as well many tinned or processed products, are full of added, hidden sugars that cause a spike in blood sugar levels.
Avoid emotional eating: try not to reach for food when you’re feeling stressed as it diverts blood flow away from your digestive system and it will probably just leave you feeling bloated and uncomfortable.
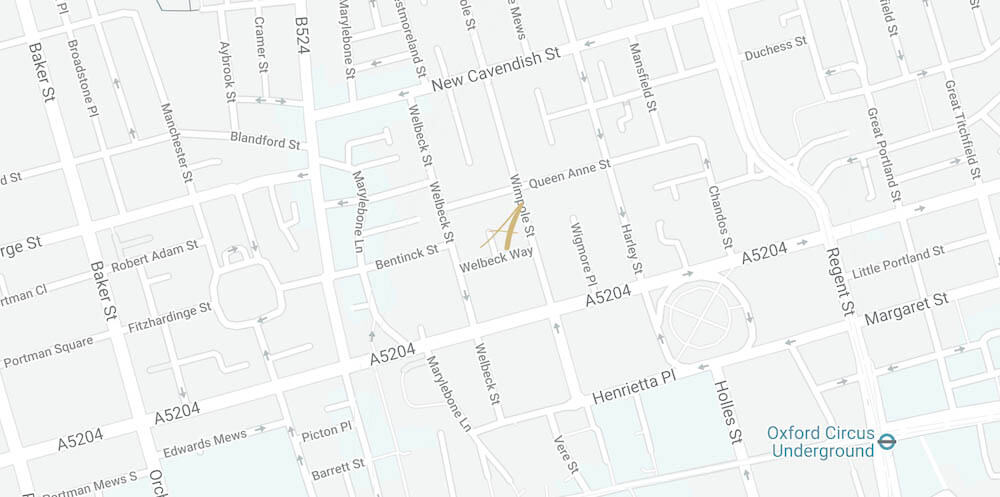
 Alex Ballard (@alextalksdiet), a Band 7 specialist fertility dietitian in the NHS, specialises in preconception nutrition and works with Aria Fertility, helping patients with general enquiries about fertility and nutrition and how that links to fertility treatment or any other health conditions
Alex Ballard (@alextalksdiet), a Band 7 specialist fertility dietitian in the NHS, specialises in preconception nutrition and works with Aria Fertility, helping patients with general enquiries about fertility and nutrition and how that links to fertility treatment or any other health conditions
“A Mediterranean diet is specifically good for mood; one with oily fish, lots of fruit and veg, nuts and seeds, and whole grains. But I find that just the act of focusing on diet and taking control can also be good for allaying anxiety as the patient is being proactive about improving their own health.”
We work closely with a wide range of practitioners to provide support throughout your fertility journey – click here to visit our Support Hub.

 Emma Cannon, a fertility and women’s health expert, is a registered acupuncturist and works with men and women who wish to optimise natural conception or support
Emma Cannon, a fertility and women’s health expert, is a registered acupuncturist and works with men and women who wish to optimise natural conception or support  At Aria, we work closely with Senior Fertility Counsellor Tracey Sainsbury who provides implications counselling for individuals and couples around all fertility issues. Implications counselling aims explore the psychological as well as the social, legal, and ethical implications around your treatment.
At Aria, we work closely with Senior Fertility Counsellor Tracey Sainsbury who provides implications counselling for individuals and couples around all fertility issues. Implications counselling aims explore the psychological as well as the social, legal, and ethical implications around your treatment.