In vitro fertilisation is a challenging time as it’s both emotionally and physically demanding, and one way to prepare for IVF is to focus on the potential benefits of improving egg quality or ovarian function through lifestyle changes, such as nutrition.
Leading fertility nutritionist Melanie Brown believes nutrition can help improve fertility.
“Women are constantly being told nothing can improve the quality of their eggs. And while we are all born with the eggs we shall ever have in our lifetimes, the environment in which those eggs mature is fundamental to their quality, so this assertion is not strictly true.
“There are many reasons why someone’s egg quality or ovarian function might not be optimal and can be positively influenced.
“We know that smoking damages egg quality, so conversely, I believe that nutrition and other lifestyle changes could also help to improve egg quality. If you can do something that adversely affects egg health, it shows they are not immune to their environment.”
IVF vs a normal menstrual cycle
During a normal menstrual cycle, many follicles containing immature egg cells or oocytes will develop and grow when your body releases a follicle-stimulating hormone called FSH.
Typically, one standout follicle grows faster than all the others, known as the dominant follicle. It sends a signal to decrease the amount of FSH being produced, which causes the other follicles to cease developing, leaving only the one dominant follicle to continue growing and the egg inside to mature.
In an IVF cycle, however, the goal is to grow multiple follicles simultaneously, a process that does not occur in a natural cycle.
“I often say to my patients, if you look at the progress of an IVF cycle as a flow chart, you can see how important it is to ensure you are as well prepared as possible,” Melanie explains. “You might have 18 follicles, which release 14 eggs, 10 of which are mature eggs, from which eight go on to be fertilised, six then go through to day three, and maybe two become day 5 blastocysts.”
Preparing for IVF with nutrition
“I can also advise patients on all the fertility-improving strategies out there on the internet – milk or no milk, soya or no soya, is DHEA right for you, how do I use melatonin?
 “There’s an ever-running argument about milk consumption during IVF. Many nutritionists think milk is the devil’s work as it’s very inflammatory and can be a factor in everything from acne to polycystic ovaries. And I certainly think that’s true for those that suffer from certain conditions.
“There’s an ever-running argument about milk consumption during IVF. Many nutritionists think milk is the devil’s work as it’s very inflammatory and can be a factor in everything from acne to polycystic ovaries. And I certainly think that’s true for those that suffer from certain conditions.
“But, if you don’t suffer from those conditions, I think there’s quite an argument for consuming milk in an IVF cycle. Milk is meant to grow baby animals and full-fat milk is full of growth factors and growth-promoting nutrients.
“Iron takes oxygen to our cells, so if you are even slightly anaemic, then it means you’re not getting enough oxygen to your ovaries. Yet, many people might be entering an IVF cycle with mild anaemia – if you have undiagnosed endometriosis, very heavy periods or have a vegetarian or vegan diet.
“A protein-rich diet is essential to support multiple follicle growth during an IVF cycle. Protein makes up the building blocks for every cell in our bodies, including our sperm and eggs. So ensuring you have the right amount of protein is essential.
“I see maximising ovarian function and potentially improving egg quality before IVF, as a ‘project’ – usually three months will do it.”
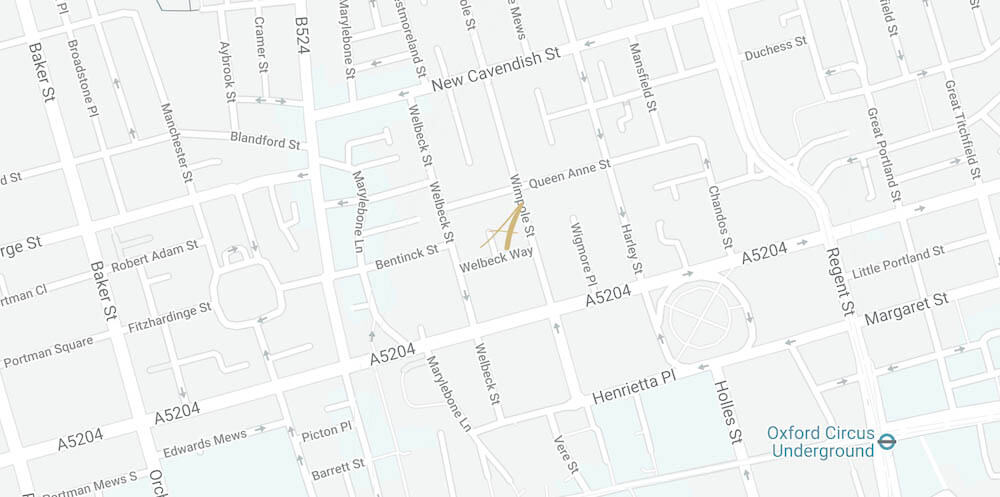
For more advice on anything fertility and nutrition-related, see Mel’s website: melaniebrownnutrition.com. Call +44 (0) 203 263 6025 or email us at admin@ariafertility.co.uk for advice on preparing for IVF.
For more information on the individual practitioners and organisations offering support, advice, and information to those undergoing fertility treatment, please visit our Support Hub.

 “I am delighted to have a chat with anyone who needs more information or just so we get to know one another. I feel it is so important to build a close relationship to my patients, so they trust in the support and advice that I give them.”
“I am delighted to have a chat with anyone who needs more information or just so we get to know one another. I feel it is so important to build a close relationship to my patients, so they trust in the support and advice that I give them.”