Egg freezing provides a unique opportunity to protect your fertility potential and it is becoming an increasingly popular and effective treatment option to preserve your eggs until you are ready to start a family in the future.
If you are contemplating egg freezing, it’s essential you are fully informed about the steps involved and the potential benefits as well as possible drawbacks. Here are just some of the questions we commonly get asked about egg freezing.
What is egg freezing?
Egg freezing is a process in which eggs are retrieved from the ovaries and cryopreserved for possible use later. As fertility declines as you age, your chances of achieving a successful pregnancy will be similar to the age you froze your eggs.
Why should you consider egg freezing?
Today, more and more women are delaying starting a family until later in life due to personal, social or career circumstances. As techniques and technology continue to evolve, egg freezing has become an increasingly popular method of preserving fertility, as freezing your eggs at a younger age may offer a better chance of a successful pregnancy.
How are eggs frozen?
Once the eggs are retrieved from the ovaries, they are assessed, and mature eggs are frozen soon after retrieval in a technique known as vitrification. This flash-freezing method means water molecules do not have time to form ice crystals, resulting in less damage when the eggs are thawed.
What can I expect during the egg-freezing process?
The egg-freezing journey typically takes approximately 14 days. As we want to collect as many mature eggs as possible per cycle, the ovaries are stimulated with hormone injections. We will perform scans and blood tests to monitor the progress so we can time the trigger injection. Egg collection is then timed for approximately 36 hours after this time.
What can I expect from the egg retrieval process?
Egg collection is done transvaginally in much the same way as a transvaginal scan. The procedure typically takes 30 minutes under mild sedation. Your eggs will be collected using a needle that goes into each ovarian follicle and uses gentle suction to pull out the fluid which contains the egg.
Once rested, you should be able to return home after a couple of hours. You may experience tiredness, bloating, mild abdominal pain and light vaginal bleeding for a few days after your procedure. Most patients can resume their regular routine the next day.
Is egg freezing painful?
Some elements of the egg-freezing process can be uncomfortable, depending on your sensitivity. However, the experience is not painful for most women.
The hormone injections can sting a bit, but your nurse will advise on how best to administer these injections. During this time, you can feel very bloated and crampy, varying from patient to patient.
Your egg retrieval will be performed under sedation so you will not feel anything, but afterwards, you may experience some mild abdominal pain and a little soreness.
What are the risks of egg freezing?
Egg freezing is considered a relatively safe, low-risk procedure. One potential risk is ovarian hyperstimulation syndrome (OHSS).
Stimulation of the ovaries is a deliberate aspect of egg freezing, as we try to obtain as many mature eggs as possible. When the ovaries are stimulated, there is a possibility of OHSS developing, which is an excessive response to the drugs used to encourage multiple follicles to form.
Most cases of OHSS are mild to moderate, occurring in up to 5% of all patients undergoing IVF treatment. This can give symptoms such as mild abdominal discomfort and nausea and usually settles with painkillers and maintaining a good fluid intake.
Very occasionally, OHSS can be more severe, causing marked swelling of the abdomen, dehydration, nausea and vomiting and difficulty in breathing. This is uncommon and may happen in up to 1% of women undergoing ovarian stimulation.
The team will manage the risk of OHSS, which might include altering the dose of stimulation medications or using a different trigger injection.
How many eggs should I freeze?
The success of techniques like IVF is dependent on two main factors: the age at which treatment takes place and the number of eggs the ovaries can produce.
With egg freezing, an additional factor to consider is the chances of eggs thawing successfully.
Current thinking is that women under 35 should try to freeze 20 eggs and women over 35 20-30 eggs. However, a woman’s ovaries may respond very differently to stimulation, which means multiple egg freeze cycles may be required to achieve this number.
How long can I store my eggs?
Once vitrified, eggs may be stored for any period up to a maximum of 55 years from the date they are first placed in storage. However, you must renew your consent every ten years; therefore, you must keep your contact details updated with us.
What happens when I’m ready to use my frozen eggs?
Your eggs will be transported from the cryostorage facility to the clinic and thawed. They will then be fertilised with partner or donor sperm using a fertility process called ICSI.
What happens next?
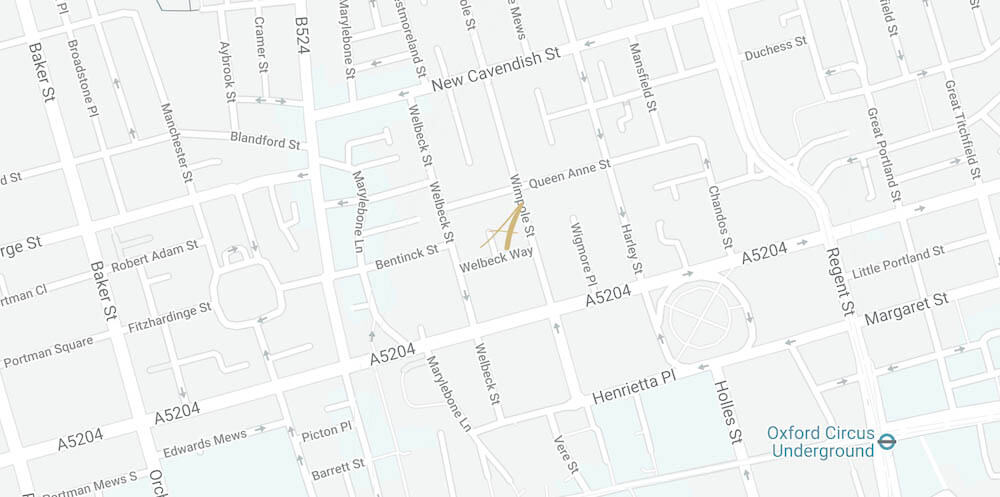
If you decide to proceed with egg freezing, the first step is a consultation with one of our fertility experts and a fertility assessment. Once any relevant investigations are completed, your consultant will discuss the results with you and any implications. They will inform you of what to expect from egg freezing and provide a detailed, fully costed treatment plan.
You will then attend a nurse planning appointment. During this appointment, we will map out the timeline of your egg-freezing treatment. They will also go through the consent process, which will be explained in detail, and your nurse will answer any further questions you may have.
When you are ready to start, you call to tell us when your period has started, and from there, the egg freezing cycle takes approximately 14 days.
If we haven’t answered your egg-freezing question, contact us to find out more.