Everything you wanted to ask an embryologist: part two
Embryologists perform an essential role throughout the patient pathway at an IVF clinic. As well as their lab work, they also regularly interact with patients. In part two of ‘Ask an Embryologist’, Senior Clinical Embryologist Kim Hill answers your most frequently asked questions, including how often you will hear from your embryologist.
“We speak to patients in general every other day, typically after the fertilisation check, then on day three and day five. Obviously, some people prefer not to hear from us during that time and just want to know the final outcome, which is fine. Some people want to speak to us every day. It depends on how the patient feels and what support they need.”
What is the difference between a day three embryo and a blastocyst?
At day 3, it should have about six to eight cells. When it becomes a blastocyst, it makes different cell types and expands. You can usually start to see a small cavity forming by the end of day four, and by day five, you would hope to see a nicely expanded blastocyst with clear cells inside. It usually reaches that stage on day five or day six, but it can even be from day 7.
Why do so many embryos stop growing after day 3 and not make it to day 5?
Most fertilised embryos reach the day 3 stage, as the egg drives development until that point. The drop-off from day 3 to day 5 is when the egg and sperm fuse, creating a new genome. This process requires a lot of energy.
If it reaches the blastocyst stage, we know it’s overcome a major hurdle in the embryo’s growth.
Only about 40 to 50% of embryos make it from fertilisation to day 5 stage, so it is essential to prepare patients for this.
Is there anything that could address this in the future?
Unfortunately, IVF is a numbers game, which is why the patients go through the stimulation process because we want to start with as high a number as possible.
Techniques will hopefully be developed in the future to address that drop-off. Artificial Oocyte Activation (AOA) with Calcium Ionophore is currently being investigated, although more research is required to determine its benefits for patients.
When my embryologist talks about normal fertilisation the day after my retrieval, what does that mean?
A newly fertilised embryo will have one small circle for the egg and one small circle for the sperm. That is what we call a Pronuclear (2PN) embryo. Sometimes, you can get a 1 PN or 3 PN embryo, and this usually indicates that something isn’t right. For example, three circles could indicate that two sperm fertilised the egg at the same time during IVF, which means there is too much genetic material in there, and it’s likely that that embryo will be abnormal.
What is assisted hatching?
Assisted hatching is a technique that we use to help the embryo hatch out of its hard outer shell. When the embryo is small, it has a thick layer of protein around it and when it’s ready to implant, it normally hatches out of this shell.
A small incision is made using a laser. Sometimes, we may do this if the embryo can’t hatch naturally, but often, we do it if we need to do a biopsy. At that point, the embryo is hundreds of cells, and this helps us get a couple of cells from the outer layer with the least manipulation as possible.
What is PGT-A?
PGT-A is pre-implantation genetic testing for aneuploidy, and more and more patients are opting for it compared to three to five years ago. It checks the number of chromosomes inside the embryo.
The Aria consultant will discuss this with them initially but often they are receiving a lot of information at this stage, so we will also discuss this with them during the decision-making process.
Can my embryo be damaged during the PGT biopsy process?
Anything that requires embryo manipulation is risky, but I would say the risk here is very low, under 5%. The process requires us to remove three to five cells from the embryo, but at this point, it has hundreds of cells, and we know it can regenerate those cells quickly as long as the quality is sufficient.
It requires quite a bit of training on our part because you are taking cells from the outside, which are the placenta cells, rather than the inner cell mass.
How is sperm quality assessed?
Sperm quality is taking a front seat compared to ten or fifteen years ago. There has been a decrease in sperm count worldwide, and there has been much research into the role of lifestyle factors, such as our sedentary lifestyle, diet, stress, and pollution.
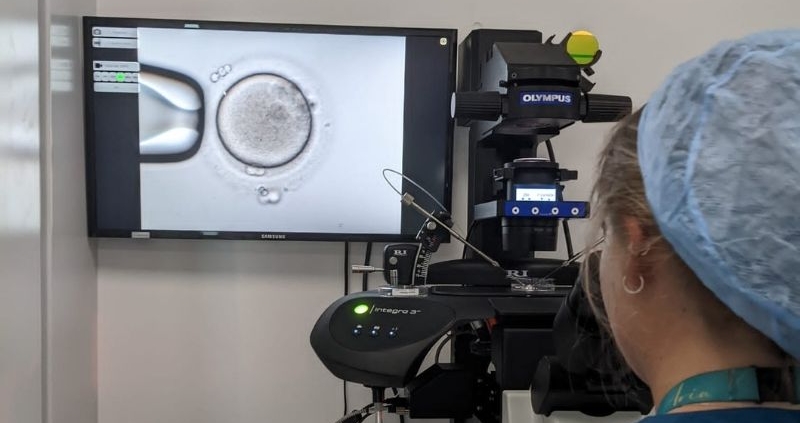
We assess the sperm under a microscope, looking at the number of cells we can see, how they move, and how they look. We use certain criteria to determine whether we can proceed with IVF confidently, knowing that there’s a good chance of fertilisation.
If it doesn’t quite meet those criteria, we recommend ICSI, which bypasses the swimming process.
How much does sperm DNA fragmentation affect the quality of embryos?
Sperm DNA fragmentation is linked with poor embryo development and quality and is being taken more seriously now. We can perform a test to determine the damage or ‘fragmentation’ of the strands of DNA held inside the sperm head. This can be genetic but can also be caused by several factors, including lifestyle choices, environmental factors, and health issues.
More questions? Call +44 (0) 203 263 6025 or email us at admin@ariafertility.co.uk to arrange a consultation at Aria Fertility.