A question of balance: understanding hormones and fertility
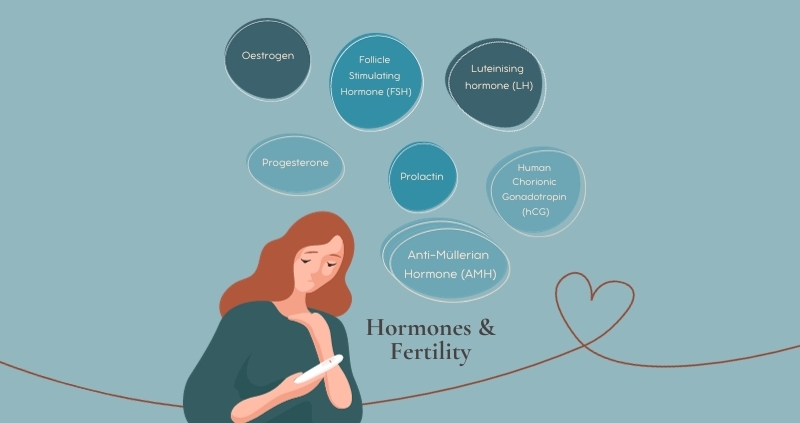
Women have a complex, interconnected hormone network that can impact fertility.
Hormones are chemicals primarily produced in the endocrine glands, and they act as messengers that control and influence different bodily functions, including conception and pregnancy.
A hormonal imbalance is when your body produces too much or too little of a particular hormone. Conception relies on a carefully choreographed mix of hormones produced in a specific sequence during the menstrual cycle so that a small change can disrupt the hormones and fertility process.
In our latest blog, we discuss the 7 major fertility hormones that are at play when trying to conceive:
Hormones and fertility
1 Oestrogen
Oestrogen is the primary female hormone; it kickstarts puberty and continues to regulate the menstrual cycle, among many other essential bodily functions. Produced by the ovaries and placenta, it maintains the uterine lining and regulates other key fertility hormones.
2 Progesterone
Mainly made in the ovaries, progesterone helps regulate your menstrual cycle, and after ovulation, it helps the uterine lining to become receptive to the implantation of a fertilised egg. It also prevents the uterine muscles from contracting so the egg is not rejected. Low progesterone levels are thought to play a role in recurrent miscarriage.
3 Follicle stimulating hormone (FSH)
The pituitary gland in the brain makes this hormone and signals the ovaries to grow eggs. It also stimulates oestrogen production at this stage, which is necessary for the body to produce a surge of luteinising hormone (LH), leading to ovulation. This also has an impact on the cervical mucus. When ovulating, the cervical mucus changes from thick and white or creamy to stretchy and clear, which helps the sperm survive and fertilise the egg.
4 Luteinising hormone (LH)
Another hormone produced by the pituitary gland, LH works in concert with FSH. LH levels must rise just before ovulation to trigger the release of the egg from the follicle. An imbalance in LH is often a cause of irregular menstruation.
5 Human chorionic gonadotropin (hCG)
Often known as the pregnancy hormone, hCG is only produced by the body when you’ve conceived. hCG levels rise just after conception until about ten weeks in pregnancy, and it’s this chemical that pregnancy tests detect and measure. It tells the body to stop menstruation and helps thicken the uterine lining to support the growing embryo
6 Prolactin
Made by the pituitary gland, prolactin is a critical player in regulating your menstrual cycle. An imbalance in prolactin, especially if produced in excess, can cause menstrual and fertility problems.
7 Anti-Müllerian Hormone (AMH)
AMH is produced in the ovarian follicles and is responsible for maintaining your body’s immature eggs and regulating the number of growing follicles and their selection for ovulation. If you’re undergoing IVF, measuring the levels of AMH can be used to estimate your ovarian reserve
AMH remains consistent throughout your menstrual cycle, whereas other hormones fluctuate. For this reason, we can test your AMH level at any point during your process and this will provide us with an indicator of your current reproductive potential. If the level of your AMH is low, this does not necessarily mean you will not be able to conceive.
AMH levels strongly correlate with the antral follicle count (AFC), and when combined, we can provide you with a clearer understanding of your fertility. Get in touch to arrange your Female Fertility Investigation at Aria Clinic.
Call +44 (0) 203 263 6025 or email us at admin@ariafertility.co.uk.